In a large meta-analysis that compared the effects of selective serotonin reuptake inhibitors (SSRIs) against various forms of exercise, a team of researchers determined that nearly all common forms of physical activity display a greater potential for improving symptoms of depression than the flagship antidepressant medication.
This included dancing, yoga, running, walking, jogging, cycling, “mixed aerobic exercise,” weight training, and tai chi/qi gong. While the risk of bias was determined to be high in many of the component analyses, the study, published in the British Medical Journal, contained interesting granular findings that should be considered for anyone who knows someone struggling with depression.
SSRIs have an interesting literature attached to them. In 1988, the United States was first introduced to this class of psychiatric medication with fluoxetine, aka Prozac, manufactured by Elly Lilly. Five other drugs followed, and by 2004, total Medicaid spending on SSRIs and a similar class of drug called SNRIs had grown to $2 billion every year.
Like all mass-prescribed pharmaceutical products, skepticism and criticism of their use followed. For reasons that some physicians have suggested are financially motivated, SSRIs continued to be prescribed in huge numbers long after a case had been built that they significantly increased the risk of psychotic episodes, and that some of their manufacturers worked to hide this in data sets submitted to regulatory bodies and scientific journals.
In a controlled trial of two SSRIs called paroxetine and clomipramine sponsored by GlaxoSmithKline, 75% of the subjects had an adverse effect on paroxetine, 21% had a severe adverse effect, and 13% committed a suicidal act which amounted to 1 in 8 subjects.
In a 2009 review of the literature, Joel Kaufman, Ph.D. wrote:
Early findings of severe adverse effects by SSRI makers came to light only after the class was established. Of 53 healthy volunteer studies on fluoxetine, the results of only 12 were openly reported. From 35 healthy volunteer studies on paroxetine, pre-launch, the results of only 14 appeared. From 35 pre-launch healthy volunteer studies on sertraline, only seven appeared.
Among [these] unpublished trials, there was one in which all volunteers dropped out because of agitation (akathisia). In published work on sertraline, data excluded material on behavioral toxicity, including at least one suicide of a healthy volunteer, and in a different trial, 2 of 20 volunteers became intensely suicidal. Yet as early as 1986, clinical trials showed a rate of 12.5 suicides per 1,000 subjects on fluoxetine vs. 3.8 on older non-SSRIs vs. 2.5 on placebo.
As simple as movement
The authors of the BMJ analysis, who represent over a dozen Australian medical and research institutions, hoped to identify the optimal dose and modality of exercise for treating major depressive disorder, compared with psychotherapy, antidepressants, and control conditions.
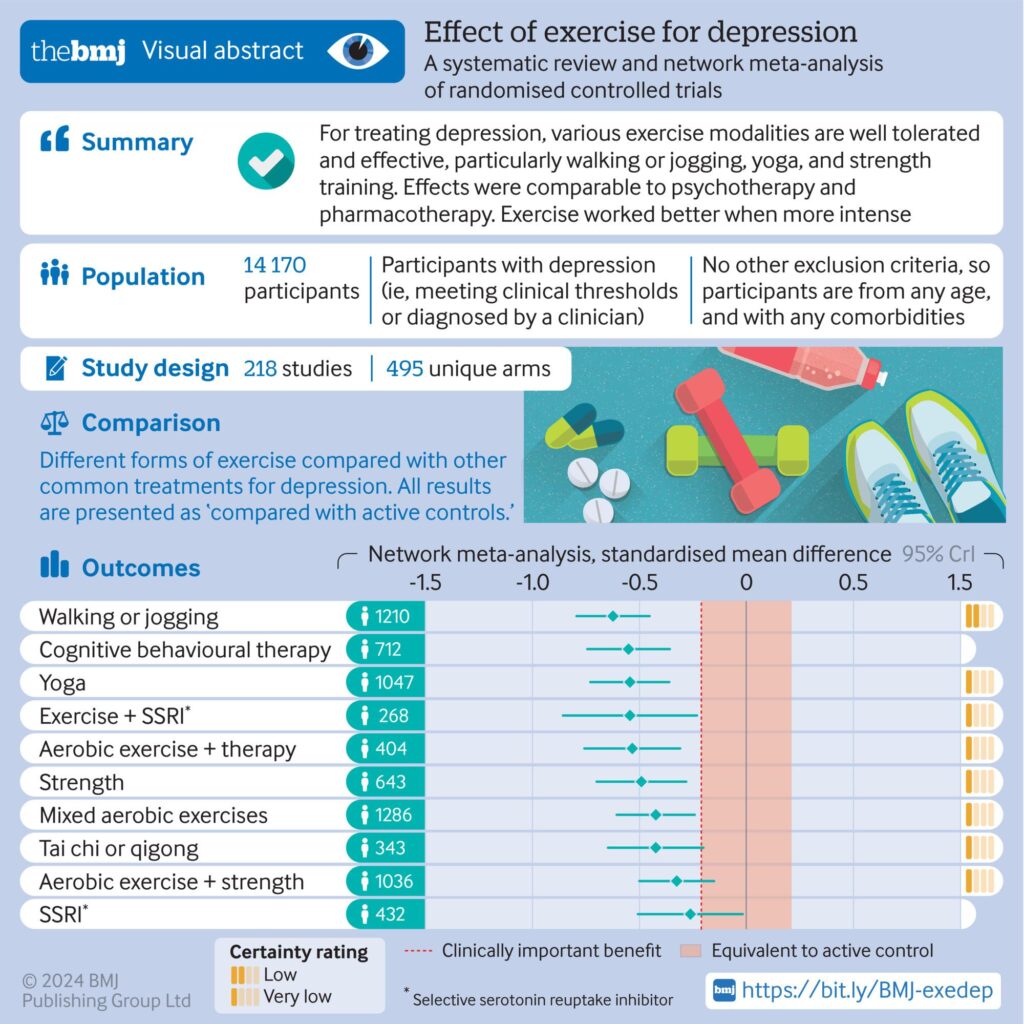
Risk-of-bias assessments were conducted by the team, rather than relying on assessments reported in the studies themselves—which were all at least randomized, but were not double-blinded. In total, 218 studies representing over 14,000 participants were included.
“Major depressive disorder is a leading cause of disability worldwide and has been found to lower life satisfaction more than debt, divorce, and diabetes, and to exacerbate comorbidities, including heart disease, anxiety, and cancer,” the authors state. “Exercise is an effective treatment for depression, with walking or jogging, yoga, and strength training more effective than other exercises, particularly when intense”.
“Yoga and strength training were well tolerated compared with other treatments. Exercise appeared equally effective for people with and without comorbidities and with different baseline levels of depression,” they concluded in their introduction.
However, dancing was by far and away the most effective method of exercise, which isn’t surprising since it coalesces around several situations that are known to improve mental well-being: social contact, physical human-to-human contact, and live music.
Each form of exercise was compared to an active control and SSRI use. Plotted with markers for clinically significant benefits, some interesting comparisons can be drawn.

Digging down
Like all effects attempting to be observed in humans through science, there was a spectrum representing the mean, highest, and lowest recorded effects seen in the data. For example, the highest end of the spectrum of SSRI benefits was equal to or less than dancing, walking, jogging, yoga, aerobic therapy, and strength training, while the mean effect of the antidepressants was lower than everything apart from “physical activity counseling”.
The mean effect of dancing was greater than the highest observed effect for anything else. An interesting column entry was ‘exercise + SSRI use,’ which while having a mean as high as yoga, and an upper end as high as the upper end of walking or jogging (the second most effective activity overall), the lower end was dramatically lower than the lower ends of all other exercises, and fell even below the level of clinically significant benefit.
Of all the exercises, only tai chi/qi gong, a mixed program of aerobic and strength training, and cycling had lower ends that fell beneath the clinically significant marker.
Other interesting particulars were discovered in the data. A dose-dependent response curve was clearly and consistently observed for the intensity of exercise prescribed, although walking and jogging was still the second most effective activity, suggesting it probably had a greater cognitive element than other exercises.
There was no indication that participants were likely to relapse within the measurement period, and effects remained steady when measured either directly after the intervention or up to six months later. Contrary to expectations, studies describing a level of participant autonomy (i.e. choice over frequency, intensity, type, or time) tended to show weaker effects, suggesting that accountability to a trainer or the presence of social support within a group activity would improve exercise as a treatment plan.
Nevertheless, some interventions were better delivered in groups (yoga) and some were better delivered individually (strength training, mixed aerobic exercise). Yoga was particularly effective among men, while strength training was particularly effective among women.
“Although confidence in many of the results was low, treatment guidelines may be overly conservative by conditionally recommending exercise as complementary or alternative treatment for patients in whom psychotherapy or pharmacotherapy is either ineffective or unacceptable,” the authors posit in their conclusions.
In a separate, 2022 analysis and review, most double-blinded, placebo-controlled studies were found to show no evidence of reduced serotonin activity in people with depression compared to people without. So while the results might have low confidence, the basic theory underlying SSRI prescription—that serotonin content and uptake is lower in the brains of depressed people—may have no basis anyway. WaL



