Among individuals who prefer to form their eating patterns around maximizing nutrient intake, there’s an urge to proclaim that, as Hippocrates said, let thy food be thy medicine. And why it’s true that spinach probably won’t help someone suffering from blood sepsis, for example, there are many common causes of hospitalization for which a nutrient deficiency of some kind is almost guaranteed to be present.
The bridge to believing that a kiwi is somehow the same as a doctor-prescribed medication or something delivered in a clinic via a syringe can be difficult to cross for people, doctors included. It’s difficult to know how often it happens that a primary care physician orders a test for nutrient levels in America. Older adults are generally encouraged to get their blood work done, but it’s more likely to be examined for signs of cancer, triglycerides, or LDL cholesterol particles.
But doing so more often could save lives and potentially billions in hospital bills, since inadequate nutrient intake is not just a risk factor, but has been found to place people as high as the 90th percentile for the risk of things like pneumonia, COVID-19, Diabetes Miletus, Osteoporosis, and many others.
Almost without variation, the studies cited below include a note on the patients’ inadequate vitamin D status.
COVID-19
During 2020 and 2021, the Western world was seized by a collective hysteria during which the norms relating to infectious diseases going back through decades of medical research were seemingly burned in effigy. From 2019 back to our grandparents’ time, there have been well-understood characteristics about upper-respiratory tract infections, and one of those was that they prey more heavily on vitamin-D-deficient people.
It should have been public policy number one—to advise an increased intake of sunlight and vitamin D supplements—from the very start, and should have surprised no one when Spanish researchers found 80% of 216 COVID-19 patients at the Hospital Universitario Marqués de Valdecilla had vitamin D deficiency, nor when the Galilee Medical Center in Nahariya, Israel found that a low vitamin D status was present in 87.4% of patients with severe or critical COVID-19, but only 34.3% of patients with mild to moderate disease.
Despite that, well-known health influencer and functional medicine practitioner Chris Kresser reported in his newsletter that trying to share these studies on his social media accounts got him thrown in the sin bin.
Pneumonia
There’s an old saying in medicine “break your hip, die of pneumonia”. Pneumonia causes 2.4 million deaths a year, and nearly 65 million hospital admissions. In a study of 50 hospitalized patients with community-acquired pneumonia, 96% had an inadequate vitamin C status, 62% of whom had a clinically moderate deficiency and 22% had a serious deficiency.
Vitamin C is one of the most widely used antioxidants in the body. It enhances the killing of harmful microbes, as well as phagocytosis—the clearing of invasive particles by macrophages. At the same time, it protects host tissue from excessive damage by enhancing neutrophil apoptosis and clearance by macrophages and decreasing neutrophil necrosis.
Vitamin C, also known as ascorbic acid, comes in three forms, and while it’s known to be common in fruit, kiwi and guava contain more than 100% of the recommended daily allowance of the normal ascorbic acid, but also a small amount of dehydroascorbic acid which functions differently in the body and is rarer to find.
Diabetes
In a study of 116 type-2 diabetes patients, vitamin D was found to be deficient in 86% of them. The study took a look at several different minerals and suggested that several of them could play a prominent role in the disease.
Osteoporosis
A large review of osteoporosis and osteopenia found that, once again, vitamin D status played a significant role in the health outcomes of especially older women living with this disease. One study done in Colombia found 55% had a vitamin D deficiency, while a literature review done in America put the number at 66%.
These bone conditions are well-studied and one of those areas where nutritional science may come into regular conversation between a patient and a doctor, particularly as it relates to calcium.
In 1994, estimated RDAs of calcium in women ranged around 570 mg per day, but only 1% of those over age 50 were reported to consume this recommended intake.
Sepsis
To return to the contrarian example previously cited, one study found that 71% of patients that suffered septic shock had a clinical-level thiamine deficiency. Also known as vitamin B1, thiamine is a critical part of the citric acid cycle, one of the three prime metabolic processes that generate energy in the body.
Like good scientists, the authors noted that it’s unclear whether the deficiency contributed as a cause or was a consequence of the sepsis, however thiamine’s work in the citric acid cycle helps avoid unnecessary production of lactic acid in the muscle tissues which would worsen sepsis.
Reviewing the sepsis literature with an eye on vitamin D, the researchers found that vitamin D insufficiency was reported in between 100% and 79% of all sepsis patients.
A variety of cancers
In a meta-analysis looking at vitamin D status and breast cancer, the researchers found totals varying from 23% to 96% of new breast cancer diagnoses came with a vitamin D deficiency. Regarding colorectal cancer, the second-most common form of cancer worldwide, 14 studies of the highest quality totaling over 100,000 Germans with colorectal cancer found that 59% were diagnosed with vitamin D3 deficiency.
In a review looking to see if vitamin D status predicts bone tumor malignancy, the NIH found that 83% of patients who were diagnosed with a malignant bone tumor had insufficient vitamin D levels.
In a randomized trial of children with pediatric cancers of various kinds, 96% of the 23 children in the trial had more than one dietary nutrient deficiency, while 36% had more than three.
Migraines
While no one in the throes of a migraine headache is rushing to their kitchen, a study of 7,800 children who suffer from migraines found that 83% of them were deficient in various levels of Coenzyme Q10, also called ubiquinone—found in fatty fish, beef, peanuts, spinach and more.
In folate, also known as vitamin B9, 59% were below the level at which a supplement is recommended, while 67% were not getting enough riboflavin (B2).
More to say
There is plenty more that could be said here, but the lengths to which this investigation could continue are essentially beyond what anyone has time to read or research personally, since many states of disease where nutrient deficiencies may play a role are simply not examined to the precise detail presented in the studies here.
Indeed there are a myriad of dysfunctions that are too general, common, or mild to be diagnosed or even to receive much attention from the person suffering from them, like muscle stiffness, cough, dry eyes, fatigue, or upset stomach, all of which may have hidden nutritional underpinnings.
Additionally, there are conditions in which a nutrient deficiency is not a hidden contributor, but the main culprit, for example in anemia (iron), scurvy (vitamin C), or inflammatory bowel diseases like IBS, Crohn’s, and ulcerative colitis.
It’s not so much then to say that food is a cure, but for the person wanting to communicate the value of nutritional homeostasis to someone who is more likely to trust in medicine, the evidence shows that good old vitamins and minerals would be the best place to start. WaL
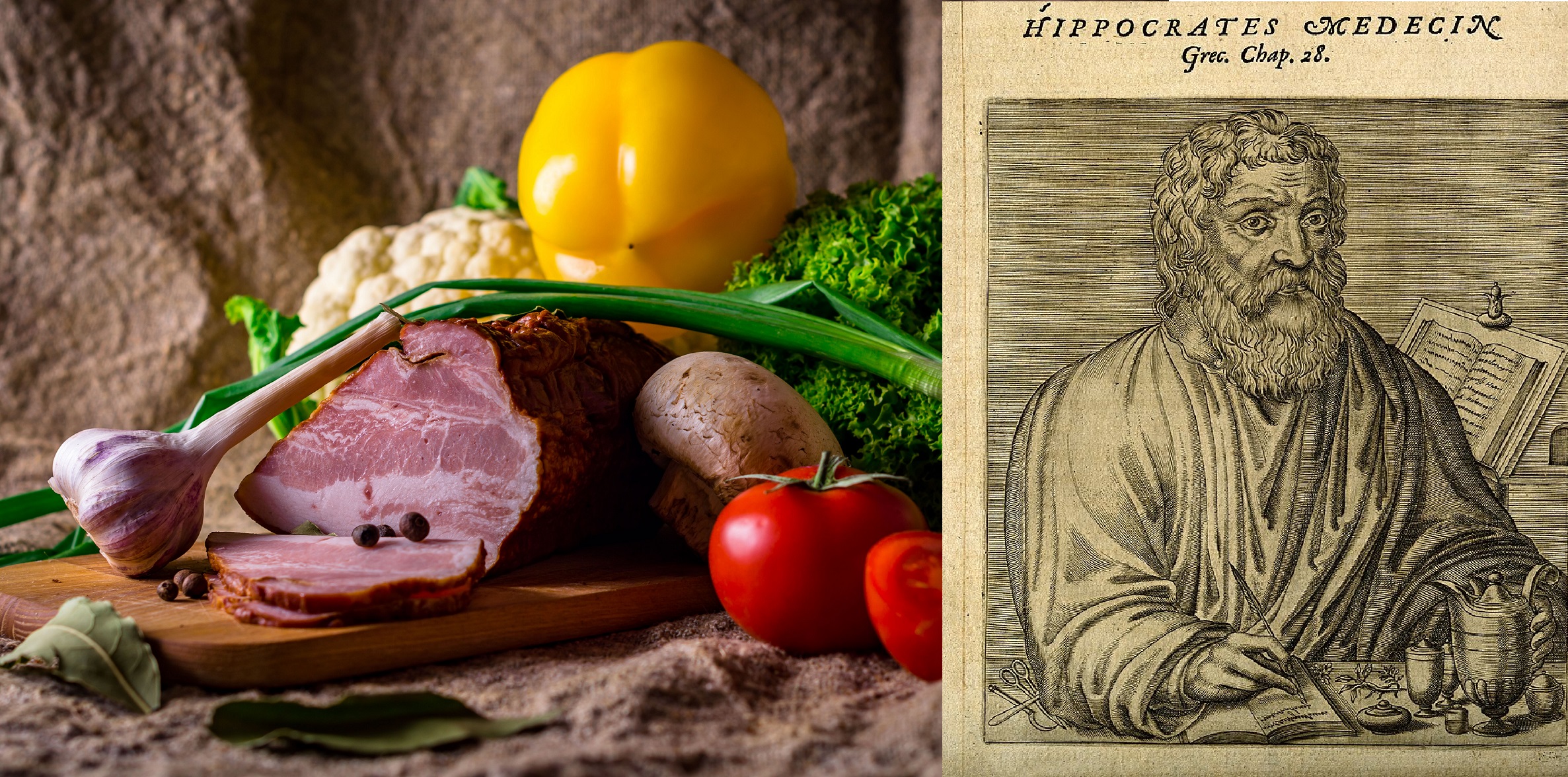
PICTURED ABOVE: The Greek physician Hippocrates said “let thy food by thy medicine”.